Esophageal Manometry for Motility Disorders
H Pylori Breath Testing
Flexible Sigmoidoscopy
Esophageal Manometry
Esophageal manometry is an outpatient test used to identify problems with movement and pressure in the esophagus that may lead to problems like heartburn. The esophagus is the "food pipe" leading from the mouth to the stomach. Manometry measures the strength and muscle coordination of your esophagus when you swallow.
During the manometry test, a thin, pressure-sensitive tube is passed through the nose, along the back of the throat, down the esophagus, and into the stomach.
H Pylori Breath Testing
The urea breath test is used to detect Helicobacter pylori (H. pylori), a type of bacteria that may infect the stomach and is a main cause of ulcers in both the stomach and duodenum (the first part of the small intestine).
H. pylori produces an enzyme called urease, which breaks urea down into ammonia and carbon dioxide. During the test, a tablet containing urea (a chemical made of nitrogen and a minimally radioactive carbon) is swallowed and the amount of exhaled carbon dioxide is measured. This indicates the presence of H. pylori in the stomach
Flexible Sigmoidoscopy
Flexible Sigmoidoscopy is a test that a doctor uses to check the inner lining of your rectum and the lower part of your colon.
You may get this test if you have certain gut problems, such as abdominal pain, rectal bleeding, or changes in bowel habits. It’s also one of the tools that doctors use to check people for colon and rectal cancer.
A sigmoidoscope is a long, flexible tube that’s about half an inch in diameter. It has a tiny light and camera. A doctor uses it to view the lining of the rectum and the lower third of the colon.
Colonoscopy
Colonoscopy enables your doctor to examine the lining of your colon (large intestine) for abnormalities by inserting a flexible tube as thick as your finger into your anus and slowly advancing it into the rectum and colon. If your doctor has recommended a colonoscopy, this brochure will give you a basic understanding of the procedure - how it's performed, how it can help, and what side effects you might experience. It can't answer all of your questions since much depends on the individual patient and the doctor. Please ask your doctor about anything you don't understand.
Your doctor will tell you what dietary restrictions to follow and what cleansing routine to use. In general, the preparation consists of either consuming a large volume of a special cleansing solution or clear liquids and special oral laxatives. The colon must be completely clean for the procedure to be accurate and complete, so be sure to follow your doctor's instructions carefully.
Most medications can be continued as usual, but some medications can interfere with the preparation or the examination. Inform your doctor about medications you're taking, particularly aspirin products, arthritis medications, anticoagulants (blood thinners), insulin or iron products. Also, be sure to mention allergies you have to medications. Alert your doctor if you require antibiotics prior to dental procedures, because you might need antibiotics before a colonoscopy as well.
Colonoscopy is well-tolerated and rarely causes much pain. You might feel pressure, bloating or cramping during the procedure. Your doctor might give you a sedative to help you relax and better tolerate any discomfort. You will lie on your side or back while your doctor slowly advances a colonoscope through your large intestine to examine the lining. Your doctor will examine the lining again as he or she slowly withdraws the colonoscope. The procedure itself usually takes 15 to 60 minutes, although you should plan on two to three hours for waiting, preparation and recovery. In some cases, the doctor cannot pass the colonoscope through the entire colon to where it meets the small intestine. Although another examination might be needed, your doctor might decide that the limited examination is sufficient.
If your doctor thinks an area needs further evaluation, he or she might pass an instrument through the colonoscope to obtain a biopsy (a sample of the colon lining) to be analyzed. Biopsies are used to identify many conditions, and your doctor might order one even if he or she doesn't suspect cancer. If colonoscopy is being performed to identify sites of bleeding, your doctor might control the bleeding through the colonoscope by injecting medications or by coagulation (sealing off bleeding vessels with heat treatment). Your doctor might also find polyps during colonoscopy, and he or she will most likely remove them during the examination. These procedures don't usually cause any pain.
Polyps are abnormal growths in the colon lining that are usually benign (noncancerous). They vary in size from a tiny dot to several inches. Your doctor can't always tell a benign polyp from a malignant (cancerous) polyp by its outer appearance, so he or she might send removed polyps for analysis. Because cancer begins in polyps, removing them is an important means of preventing colorectal cancer.
Your doctor might destroy tiny polyps by fulguration (burning) or by removing them with wire loops called snares or with biopsy instruments. Your doctor might use a technique called "snare polypectomy" to remove larger polyps. That technique involves passing a wire loop through the colonoscope and removing the polyp from the intestinal wall using an electrical current. You should feel no pain during the polypectomy.
Your physician will explain the results of the examination to you, although you'll probably have to wait for the results of any biopsies performed. If you have been given sedatives during the procedure, someone must drive you home and stay with you. Even if you feel alert after the procedure, your judgment and reflexes could be impaired for the rest of the day. You might have some cramping or bloating because of the air introduced into the colon during the examination. This should disappear quickly when you pass gas. You should be able to eat after the examination, but your doctor might restrict your diet and activities, especially after polypectomy.
Colonoscopy and polypectomy are generally safe when performed by doctors who have been specially trained and are experienced in these procedures. One possible complication is a perforation, or tear, through the bowel wall that could require surgery. Bleeding might occur at the site of biopsy or polypectomy, but it's usually minor. Bleeding can stop on its own or be controlled through the colonoscope; it rarely requires follow-up treatment. Some patients might have a reaction to the sedatives or complications from heart or lung disease. Although complications after colonoscopy are uncommon, it's important to recognize early signs of possible complications. Contact your doctor if you notice severe abdominal pain, fever and chills, or rectal bleeding of more than one-half cup. Note that bleeding can occur several days after the procedure.
Colon Cancer Screening
A screening test is used to look for a disease when a person doesn’t have symptoms (When a person has symptoms, diagnostic tests are used to find out the cause of the symptoms.)
Colorectal cancer almost always develops from precancerous polyps (abnormal growths) in the colon or rectum. Screening tests can find precancerous polyps, so that they can be removed before they turn into cancer. Screening tests can also find colorectal cancer early, when treatment works best.
Regular screening, beginning at age 50, is the key to preventing colorectal cancer. The U.S. Preventive Services Task Force (USPSTF) recommends that adults age 50 to 75 be screened for colorectal cancer. The USPSTF recommends that adults age 76 to 85 ask their doctor if they should be screened.
You should begin screening for colorectal cancer soon after turning 50, then continue getting screened at regular intervals. However, you may need to be tested earlier than 50, or more often than other people, if—
- You or a close relative have had colorectal polyps or colorectal cancer.
- You have an inflammatory bowel disease such as Crohn’s disease or ulcerative colitis.
- You have a genetic syndrome such as familial adenomatous polyposis or Lynch's Syndrome
Upper Endoscopy
EGD is a test to evaluate the lining of the esophagus, stomach, and duodenum using a thin, flexible tube called an endoscope. It is usually done to evaluate heartburn, reflux, upper abdomen pain, difficulty swallowing, persistent nausea or vomiting, ulcers, upper GI tract bleeding, black stools, anemia, weight loss, tumor of the esophagus, stomach, or duodenum, H. Pylori infection, Celiac Disease, hiatal hernia, and gastritis. During the test, your doctor may obtain a biopsy of the lining to evaluate both benign and/or cancerous growths. Biopsy can also be done to test for an infection of the stomach called H. Pylori, which can cause chronic inflammation or ulcers. Sometimes the test may be done to treat problems of the Upper GI tract such as esophagus stricture or narrowing. The EGD is then done to dilate the esophagus. Another indication may also be to remove foreign bodies blocking the esophagus
The best and safest way to evaluate the mucous lining is to have an empty stomach, so you will be asked not to eat or drink anything after midnight. You may also be asked to stop taking Aspirin, certain arthritis medicines, or blood thinning medicines for a few days prior to the procedure. If you are on blood pressure, heart, or diabetes medicines, or iron products, you will need to speak with your doctor regarding the use of these medications in the days prior to the procedure. You will need to remove all dentures and also notify the nurse of any loose or diseased teeth.
What happens during an upper Endoscopy? You will be sedated to help you relax and your doctor may spray your throat with a local anesthetic. You will then be turned to your side and the doctor will pass the endoscope through your mouth and into the esophagus, stomach, and duodenum, viewing the lining. Biopsies will be taken as needed, but you will not feel any discomfort. After the test, you may not have any memory of the procedure, even after the sedation wears off. You may, however, feel a little bit bloated because of the air introduced during the procedure and may also have a mildly sore throat for a short duration. You should be able to eat immediately following the test unless instructed otherwise by your doctor. The doctor will discuss the findings after the effects of sedation wear off. For the biopsy results, you will have to call the office 7 days after the procedure. The sedation given during the procedure will impair your judgement and reflexes, so you cannot drive for the rest of the day, even if you feel alert enough.
Complications are rare, especially when trained and experienced doctors perform this procedure. Bleeding from the biopsy site, or the site where a polyp is removed can occur, but is usually minimal. There is an extremely small risk of a hole or perforation of the esophagus, stomach, or duodenum which will require surgery to fix. You may have a reaction to the medicine/sedation drug during the procedure which can cause apnea (not breathing), respiratory depression, low blood pressure, slow heartbeat, loss of a loose tooth, or spasm of the larynx. The risk, however, is less than 1/1000 people.
Colon Polypectomy
Polyps are noncancerous tumors involving the lining of bowel, most commonly the colon. They can be flat or grow on a stalk protruding into the lumen. They can vary in size from diminutive to several centimeters in size.
Major risk factors for developing polyps are age older than 50 years, personal and/or family history of colon polyps and/or colon cancer and some rare familial polyp or cancer syndromes.
Most polyps do not cause symptoms. Large polyps can cause blood in stool. Therefore the best way to detect polyps is by screening an individual with no symptoms. Several screening techniques are available: testing stool specimen for traces of blood, sigmoidoscopy to look into left (lower one third) colon and radiological tests like Barium enema and CT colonography. If one of these tests suspects or finds polyps, a colonoscopy is recommended to remove them.
Many experts recommend a colonoscopy as a screening method for colon cancer. An advantage of colonoscopy over other screening techniques is that polyps in the entire colon can be removed during the same procedure.
Two common types of polyps are hyperplastic and adenomatous polyps (adenoma). Adenomas are considered to be the precursors for majority of colon cancers although most adenomas never become cancers. Some polyps contain small areas of cancer. Polyps cannot be differentiated into hyperplastic polyps or adenomas by the appearance. Removing all polyps found during colonoscopy is recommended. Histological (microscopic) examination of polyps differentiates between hyperplastic polyps and adenomas. Large polyps are more likely to become cancerous.
Most polyps can be removed during colonoscopy by biopsy forceps, or with wire loop (snare) with/without burning the base of polyp with electric current. A pathologist then examines the resected polyps under microscope. If a large or unusual looking polyp is removed or left for possible surgical resection, the site is marked by injecting a small amount of sterile India ink into the bowel wall. This is called endoscopic tattooing.
Possible complications (which are uncommon) of polyp resection include 1) bleeding from polypectomy site which can be immediate or delayed. Persistent bleeding is mostly controlled by treatment with repeat colonoscopy and 2) perforation of colon that may require surgical repair.
Timing of next colonoscopy depends on several factors including the number, size and the tissue type of removed polyps, personal and family history of colon polyps and colon cancer and the quality of the colon cleansing at previous procedure.
Hiatal Hernia and Heartburn
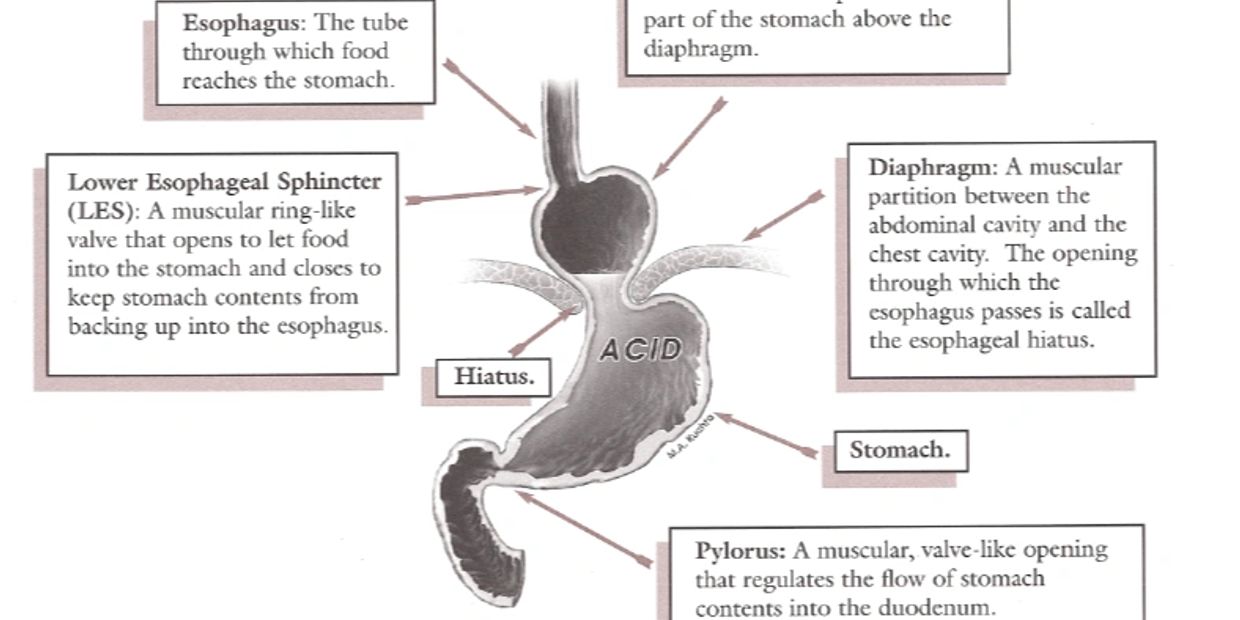
When the hiatus allows the LES and part of the stomach to protrude upward in to the chest cavity the result is a hiatial hernia. this condition is found in up to 50% of the population over the age of 50. If no symptoms are associated with it, treatment is usually not required. Frequently,however, patients with hiatal hernia also suffer from the symptom of heart burn. Heartburn is the result of stomach acid reflux into the esophagus. this occurs because of failure of the LES to close properly. When this happens, stomach contents (which ususlay contain acid ) are pushed back up into the esophagus, causing irritation and the burinning sensation commonly called "heartburn". Registration of food and bile may also occur. Heart burn can also occur without hiatal hernia.
Bravo pH Monitoring
pH, or reflux, testing is the gold standard for diagnosing GERD. And now you can test for GERD at the time of a negative endoscopy without disrupting your workflow with the Bravo™ calibration-free reflux testing system. Simply pair, place, and go. This capsule-based, patient-friendly reflux test measures acid levels in the esophagus. It has higher sensitivity than EGD and greater specificity than PPI trials, to help you obtain an objective diagnosis of GERD.
This website uses cookies.
We use cookies to analyze website traffic and optimize your website experience. By accepting our use of cookies, your data will be aggregated with all other user data.